What is a stem cell transplant?
A stem cell transplant, sometimes known as a bone marrow transplant, replaces blood-forming stem cells. The procedure can be a lifesaving option for people with blood cancers, such as leukemia, lymphoma or multiple myeloma, who do not respond to other treatment. Although stem cell transplants are still risky, the technology has improved in recent decades, and survival rates have increased. A successful transplant can put cancer into remission—often for years—and may lead to a cure.
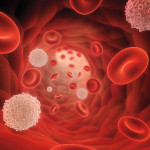
Hematopoietic stem cells are precursor cells that give rise to all the cells that make up the blood, including red blood cells, platelets and immune system white blood cells. This process occurs in the bone marrow, the spongy tissue inside certain bones.
How is a stem cell transplant done?
The transplant procedure usually involves strong chemotherapy and sometimes total body radiation—known as conditioning therapy—that wipes out existing stem cells and blood cells and makes room for new healthy ones to reconstitute the immune system.
In some cases, a patient’s healthy stem cells are collected before conditioning therapy, frozen and returned to the body afterward; this is an autologous transplant.
In other cases, the new stem cells come from a donor; this is an allogeneic transplant. Donor stem cells often produce white blood cells that can fight cancer better than the recipient’s original immune cells. The likelihood of complications is lower if the donor is a close genetic match, preferably a sibling. A compatible donor may also be found through a registry.
Stem cells may be obtained from bone marrow withdrawn from the hip bone, harvested from the blood (using drugs that move the cells from the bone marrow into the bloodstream) or collected from umbilical cord blood from newborns.
After the conditioning therapy, the new stem cells are administered via IV infusion. These cells migrate to the bone marrow, where they produce new blood cells. The initial process, known as engraftment, typically takes a few weeks, but it can take months for blood cell counts to return to normal.
What are the side effects of a stem cell transplant?
A stem cell transplant is an intensive medical procedure. The conditioning therapy kills off the recipient’s protective immune cells, so steps must be taken to prevent infections. Patients may need transfusions of red blood cells and platelets until the new stem cells can produce enough on their own. Recovery may take several months.
The conditioning regimen can cause side effects, including nausea and vomiting, hair loss and mouth sores. Some people develop cataracts, and the procedure often causes infertility. But adverse effects vary from person to person, and many are temporary.
What is graft-versus-host disease?
One potentially serious complication of allogeneic transplants is graft-versus-host disease (GVHD), which occurs when the new immune cells produced by donor stem cells recognize the recipient’s body as “foreign” and attack healthy tissue.
Acute GVHD may develop within the first few months after a transplant, often affecting the skin, gastrointestinal tract or liver. Chronic GVHD starts later and lasts longer. Steroids, other immunosuppressant medications and certain targeted therapies can be used to prevent and manage GVHD.
How can I become a stem cell donor?
Healthy people can become stem cell donors, and donors from minority groups are especially needed. Bone marrow may be withdrawn from the hip bone with a needle while the donor is under general anesthesia or stem cells may be harvested from the blood. The procedure is generally safe for the donor and could save someone’s life.
To learn more, visit Be the Match (www.BetheMatch.org) or call 800-MARROW-2.
Last Reviewed: April 26, 2021